In response to the pacing threat posed by the People’s Republic of China, the United States is preparing to defend the homeland and deter aggression.1 This future threat will be different than those seen in Operation Enduring Freedom, Operation Iraqi Freedom, and Operation Inherent Resolve. During these operations, the Air Force Medical Service (AFMS), as part of the military health system (MHS), was responsible for the historically unprecedented survivability of combat casualties.2 Numerous lessons have been learned in the recent conflicts that must be preserved. Which lessons, though, are a matter of debate as the threat of peer-on-peer conflict increases. 3 The Air Force must ensure a ready force for the next fight and not the last, otherwise the historical pattern of peacetime declines in preparedness and medical quality is doomed to repeat itself.4 This article discusses the military health system and the force makeup and skills required for the next conflict.
Brief History - Air Force Medical Service
The MHS is required to support the medical readiness of the armed forces and the readiness of medical personnel.5 In addition to this requirement, the MHS is required to provide health care where civilian health care facilities are unable to support the health care needs of members of the armed forces and covered beneficiaries. The AFMS mission is to ensure a medically fit force, provide expeditionary medics, and improve the health of all personnel it cares for to meet the nation’s needs.6
The birth of the military health system can be traced to 1956 with the passage of the Dependents’ Medical Care Act, which provided care to military and other specific beneficiaries.7 The MHS target population was relatively young and healthy. As healthcare improved and life expectancy increased, this demographic skewed older and care became more expensive. With the rising financial burden of an older population and military spending needs elsewhere, the Department of Defense created Tricare and the Defense Health Agency to, in part, stabilize costs by sharing services between military medical departments and transferring DoD healthcare to private-sector providers when appropriate.8 In addition to direct patient costs, the MHS maintains a network of 49 hospitals, 465 ambulatory care centers, and 192 dental clinics.9 This extensive network of facilities serves primarily to care for beneficiaries as part of the social contract between the military and its members since adoption of the all-volunteer force.10
The MHS is one of the largest DoD expenditures, but multiple studies reveal it has failed to sustain readiness requirements.11 This readiness gap is recognized, however, and is now being mitigated through partnerships with civilian institutions. These partnerships provide medical personnel experiences involving the highest acuity of care and in greater volumes than can be experienced in the MHS.12 As multiple examples nationwide attest, the Air Force Medical Service has been on the forefront of this move to achieve readiness through civilian partnerships.13 While these partnerships are an excellent example of what is possible, they leave costly legacy personnel and facilities.
A future AFMS as part of the MHS should retain a force that mirrors the needs of the expeditionary environment. There are limits to the clinical currency provided by beneficiary care and the opportunities provided in the civilian sector. The Air Force should focus primarily on providing personnel and skills necessary for the expeditionary environment.
Future Force Structure
The Air Force Medical Service structure and skills should reflect the requirements of the expeditionary environment. This environment is resource-limited, and the ability to evacuate patients is subject to operational considerations. Most service members with clinically taxing, chronic conditions are screened out prior to deployment, and the population is predominantly young.14 While the combat casualty is the unique patient of war, medical care required in an expeditionary setting is broad. Between January 1, 2017, and December 31, 2021, 756 US personnel were wounded in action, but there were 887,358 inpatient and outpatient encounters and 5,980 non-Covid evacuations for disease nonbattle injury, requiring 71 different specialties at role 4 facilities, also known as definitive care hospitals.15
Combat casualties will change based on operational tempo, but disease nonbattle injury will be a population and location-dependent variable. This environment differs considerably from the in-garrison environment that relies on a resource-rich network with specialty care to manage a diverse set of patients. In an expeditionary environment, the generalist performs multiple roles and is the key provider able to stabilize and care for individuals until subspecialist skills are available.
The active-duty component should be viewed as a ready force able to meet immediate military operational requirements. The force should predominantly comprise generalists capable of stabilizing a diverse set of conditions. The conditions generalists cannot manage should be evacuated to specialty care when needed. The needs in the expeditionary environment are numerous with broad categories of illness (tab. 1).16
Table 1: Proportion of disease nonbattle injury occurring in the USCENTCOM area of responsibility between January 1, 2017, and December 31, 2021 (categories of disease defined and data provided by Armed Forces Health Surveillance Division)
|
Disease Category
|
Proportion of Outpatient Encounters
|
|
Blood disorders
|
0.1%
|
|
Cardiovascular diseases
|
1.2%
|
|
Conditions arising during the perinatal period
|
0.0%
|
|
Congenital anomalies
|
0.1%
|
|
Diabetes mellitus
|
0.0%
|
|
Digestive diseases
|
2.1%
|
|
Endocrine disorders
|
0.2%
|
|
Genitourinary diseases
|
2.4%
|
|
Headache
|
1.9%
|
|
Infectious and parasitic diseases
|
4.6%
|
|
Injury and poisoning
|
28.2%
|
|
Malignant neoplasms
|
0.0%
|
|
Maternal conditions
|
0.0%
|
|
Mental disorders
|
6.9%
|
|
Metabolic and immunity disorders
|
0.2%
|
|
Musculoskeletal diseases
|
17.9%
|
|
Neurologic conditions
|
4.9%
|
|
Nutritional disorders
|
0.1%
|
|
Oral conditions
|
0.6%
|
|
Other neoplasms
|
0.3%
|
|
Respiratory diseases
|
1.6%
|
|
Respiratory infections
|
6.5%
|
|
Sense organ diseases
|
3.5%
|
|
Signs and symptoms
|
10.7%
|
|
Skin diseases
|
5.9%
|
Physicians trained in primary care specialties, emergency medicine, and general surgery are perfect for this role. They can return patients to duty without evacuation and can stabilize, hold, and transport resource-intensive patients to specialists outside the conflict zone. If additional capacity is available to provide specialty care in the expeditionary setting, then psychiatrists could also be prioritized given that mental health is the top reason for medical evacuation (fig. 1). Ideally, the AFMS personnel makeup should match the makeup of the expeditionary categorical needs (fig. 2).

Figure 1: Relative need for specialties of evacuated personnel from USCENTCOM between January 1, 2017, and December 31, 2021
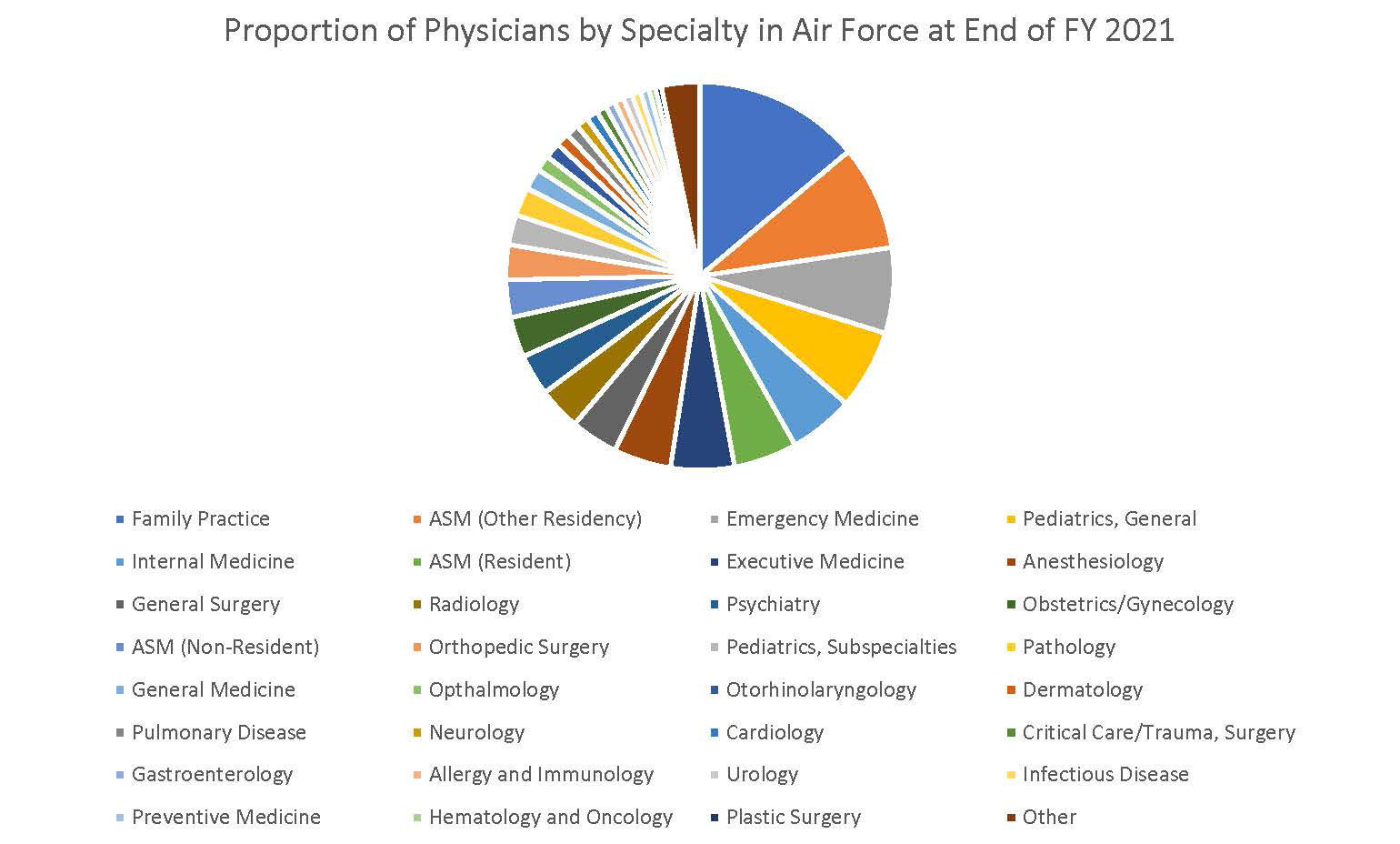
Figure 2. Proportion of physicians by specialties within the Air Force at the end of FY 2021 (data from Health Manpower Personnel Data System, 2021)
Air Force Medical Service facilities should improve their ability to provide skill-sustaining experiences relevant to the expeditionary setting. Military medical centers can reflect the expeditionary environment as demonstrated by trauma facilities such as San Antonio Military Medical Center and Navy Medical Center Camp Lejeune. These centers allowed military medical personnel to treat civilian trauma victims, providing diverse, high acuity experiences and serve as models for other military facilities. Yet not all facilities share the same constellation of circumstances. In many locations, military treatment facilities are positioned near robust civilian centers, making the military facility largely redundant. In these cases, the AFMS should partner with civilian centers with the greatest diversity of high patient volume and highacuity patients. In all cases, AFMS should focus on providing generalists with diverse caseloads to prepare for the expected diversity of the expeditionary setting.
All medical forces should continuously focus on readiness. Skill utilization should reflect the conditions and diseases that occur in a deployed environment.17 For skill sustainment, continuous experience is the ideal. Data proving when medical providers lose skills does not currently exist, but studies show that with more practice, complications decline.18 Constant practice promoting readiness is intuitive, though, just as Air Force pilots maintain skills with flight time.19 This experience requirement has been recognized by the Air Force, which offers multiple courses that provide just-in-time training or short experiences for medical personnel.20 Unfortunately, the benefit to the student is variable, and the duration of effect is unknown. What is likely true is that the embedded personnel teaching these courses have experienced the conditions most reflective of the type of combat casualties seen in conflict zones.21
Conclusion
The Air Force Medical Service and military health system has a track record of success, but past success is not necessarily going to translate into excellence at the start of the next conflict. The service must continually practice with an expeditionary mindset to maintain excellence and reduce the historical negative peacetime effect. The Air Force must prioritize generalists needed in the expeditionary environment, place personnel in expeditionary skill-sustaining facilities, and concentrate remaining AFMS facilities on sustaining expeditionary readiness in addition to conducting routine healthcare. Military medicine will thus be primed for success, and with a focus on the next conflict, practitioners and the MHS will continue to provide excellent care.
Andrew Hall
Lieutenant Colonel Andrew Hall, USAF, is the US Central Command trauma medical director.
Matthew Hanson
Colonel Matthew Hanson, USAF, is the Air Force Special Operations Command surgeon.
1 US Department of Defense (DoD), “Fact Sheet: 2022 National Defense Strategy,” DoD (website), March 28, 2022, 1–2, https://media.defense.gov/.
2 Robert L. Mabry and Robert DeLorenzo, “Challenges to Improving Combat Casualty Survival on the Battlefield,” Military Medicine 179, no. 5 (2014): 477–82, https://doi.org/.
3 Cory Welt and Andrew S. Bowen, Azerbaijan and Armenia: The Nagorno-Karabakh Conflict, R46651 (Washington, DC: Congressional Research Service, January 7, 2021), https://crsreports.congress.gov/; and Gina Harkins, “Al Asad Missile Attack Nearly Killed 150 US Troops, Destroyed 30 Aircraft: Report,” Military.com, March 1, 2021, https://www.military.com/.
4 Jeremy Cannon et al., “Comprehensive Analysis of Combat Casualty Outcomes in US Service Members from the Beginning of World War II to the End of Operation Enduring Freedom,” Journal of Trauma and Acute Care Surgery 89, no. 2S Suppl 2 (2020), http://doi.org/; and A.J. Walker, “The ‘Walker dip’,” Journal of The Royal Naval Medical Service 104, no. 3 (2018), http://doi.org/.
7 Michelle Dolfini-Reed and Jennifer Jebo, The Evolution of the Military Health Care System: Changes in Public Law and DOD Regulations, CRM D0000437.A3 (Alexandria, VA: Center for Naval Analyses, July 2000), https://www.cna.org/.
8 Philip M. Lurie, Richard R. Bannick, and Elder Granger, “The Department of Defense’s TRICARE Health Benefits Program as a Critical Plank in the Federal Platform for Health Care Reform,” IDA Document NS D-3960 (Alexandria, VA: Institute for Defense Analyses [IDA], October 2009), https://www.ida.org/; and Brenda S. Farrell et al., Defense Health Care: Additional Analysis of Costs and Benefits of Potential Governance Structures Is Needed, GAO-12-911 (Washington, DC: US Government Accountability Office, September 2012), https://www.gao.gov/.
10 Alphonso Maldon Jr., et al., Report of the Military Compensation and Retirement Modernization Commission: Final Report (Washington, DC: Military Compensation and Retirement Modernization Commission, January 29, 2015), https://docs.house.gov/.
11 John Whitley et al., Medical Total Force Management: Assessing Readiness and Cost, IDA Document P-8805 (Alexandria, VA: IDA, May 2018), https://www.ida.org/.
14 US Central Command (USCENTCOM), “USCENTCOM 061600Z Jan 22 MOD Sixteen to USCENTCOM Individual Protection and Individual-Unit Deployment Policy” (MacDill AFB, FL: USCENTCOM, January 2022), https://www.centcom.mil/.
15 Chairman of the Joint Chiefs of Staff (CJCS), Joint Health Services, Joint Publication 4-02 (Washington, DC: CJCS, 2018), https://www.jcs.mil/.
16 Andrew Hall et al., “Differences in Disease Non-Battle Injury between Combatant Commands,” Military Medicine (2022), https://doi.org/.
17 “Medical Evacuations out of the U.S. Central Command, Active and Reserve Components, U.S. Armed Forces, 2019,” Medical Surveillance Monthly Report 27, no. 5 (2020), https://pubmed.ncbi.nlm.nih.gov/.
18 Juan B. Umana-Pizano et al., “Acute Type A Dissection Repair by High-Volume Vs Low-Volume Surgeons at a High-Volume Aortic Center,” The Annals of Thoracic Surgery 108, no. 5 (2019), https://doi.org/.
19 Oriana Pawlyk, “Cuts to Flight Hours Necessary as Aircraft Sustainment Costs Surge, Air Force General Says,” Military.com, June 23, 2021, https://www.military.com/.
20 Shireen Bedi, “Readiness, Trauma at Heart of C-STARS Baltimore Partnership,” Air Force Surgeon General Public Affairs, June 28, 2018, https://www.af.mil/.
21 Andrew Hall et al., “Validation of a Predictive Model for Operative Trauma Experience to Facilitate Selection of Trauma-Sustainment Military Civilian Partnerships,” Trauma Surgery and Acute Care Open 4, no. 1 (2019), https://doi.org/; and Hall et al., “Current Challenges in Military Trauma Readiness: Insufficient Relevant Surgical Case Volumes in Military Treatment Facilities,” Journal of Trauma and Acute Care Surgery 89, no. 6 (2020), https://pubmed.ncbi.nlm.nih.gov/.
The views and opinions expressed or implied herein are those of the authors and should not be construed as carrying the official sanction of the Department of Defense, the Department of the Air Force, Air Education and Training Command, Air University, or other agencies or departments of the US government.